Fast test for inherited mitochondrial disease
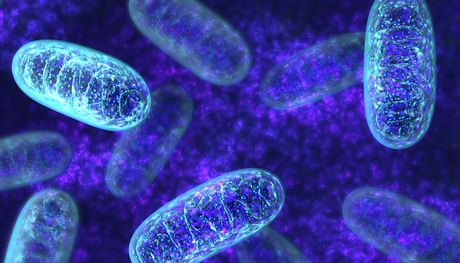
Rapid diagnosis of mitochondrial disorders is becoming a reality via a new genetic test.
The team of medics and scientists at the Wellcome Trust Centre for Mitochondrial Research at Newcastle University, together with international collaborators, have identified mutations in a gene, known as TMEM126B, involved in energy production in patients’ muscles.
Using next-generation sequencing they have now developed a rapid test which provides a result within 2–3 days — previous techniques took months.
Mitochondrial diseases affect the batteries of the cell and can lead to muscular weakness, blindness, fatal heart failure, learning disability, liver failure, diabetes and can lead to death in early infancy.
Publishing in the American Journal of Human Genetics, first author and PhD student Charlotte Alston, who is funded by the National Institute for Health Research (NIHR), describes the technique which has already identified six patients from four families affected by this form of mitochondrial disease.
She said: “Identifying a fault in Complex I, one of the building blocks of mitochondria which is responsible for causing disease combined with our custom gene capture and the latest sequencing technology, means we can screen many more genes to diagnose this debilitating disease.
“It means families can get a rapid diagnosis within days rather than the weeks and months that testing can currently take. For families who are waiting on a genetic diagnosis before trying for another baby, or they may already be expecting their next child, time really is of the essence.”
Diagnosing mitochondrial disease
Mitochondrial diseases are genetic conditions affecting the batteries of the cell, with around one in 4300 affected children born every year. Symptoms include muscle weakness, blindness, deafness, seizures, learning disabilities, diabetes, heart and liver failure. There is no cure and affected children often sadly die in early infancy.
The research has confirmed the identity of a mutation causing mitochondrial disease affecting Complex I, one of five complexes involved in energy production. The gene, TMEM126B, makes a protein necessary for assembly of the complex, with defects causing problems with energy generation in patients’ muscles.
Finding a genetic cause is important to families as it means that they can find out what is wrong with their child, enabling doctors and scientists to help them understand the risks to their future children and help prevent them losing another child.
Professor Rob Taylor from the Wellcome Trust Centre for Mitochondrial Research, who also leads the NHS Highly Specialised Mitochondrial Diagnostic Laboratory at the Newcastle Hospitals NHS Foundation Trust, said: “The diagnosis of mitochondrial disease is often a complicated and time-consuming process. There are over 1300 potential genes that can lead to disease and, as such, finding the genetic cause is sometimes like looking for a needle in a haystack.”
NHS test for affected families
Defective genes can be caused by mutations in either the maternally inherited mitochondrial genome (mtDNA) or, more frequently, the genes located on the autosomes, the 23 pairs of chromosomes which are responsible for all traits and all other genetic diseases. For a family with one child affected with this type of mitochondrial disease, there is a 25% chance of each further child being affected with the devastating condition.
Professor Taylor added: “There is sadly no cure for mitochondrial disease so rapid diagnosis means parents who are wanting to have further children can opt for prenatal testing to ensure future children are healthy and without risk of developing severe disease. It provides options for families at risk of an otherwise incurable disease.”
Highly specialised mitochondrial services are NHS funded and streamlined across the country so this genetic test is now available within routine practice to patients nationally.
This research was funded through a National Institute for Health Research (NIHR) doctoral fellowship and made possible through the Newcastle Academic Health Partners, a collaboration involving Newcastle Upon Tyne Hospitals NHS Foundation Trust, Northumberland, Tyne and Wear NHS Foundation Trust and Newcastle University. This partnership harnesses world-class expertise to ensure patients benefit sooner from new treatments, diagnostics and prevention strategies.
Originally published here.
Proteomic approach identifies new blood-clotting disorder
Analysis of lethal antibodies has helped Australian and international researchers identify a new...
Blood test for chronic fatigue syndrome developed
The test addresses the need for a quick and reliable diagnostic for a complex,...
Droplet microfluidics for single-cell analysis
Discover how droplet microfluidics is revolutionising single-cell analysis and selection in...




