Immune system boosted to fight antibiotic-resistant bacteria
Researchers from Johns Hopkins Medicine have announced an accidental discovery that could be on par with the birth of penicillin — a treatment that may provide an alternative, immune-based solution to the danger of antibiotic-resistant bacterial infections.
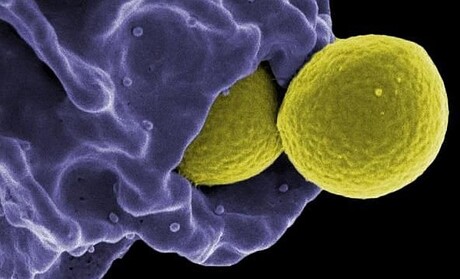
As with Alexander Fleming’s discovery of penicillin in 1928, the bacterium of note for the Johns Hopkins researchers was Staphylococcus aureus — but this time, methicillin-resistant Staphylococcus aureus (MRSA), the life-threatening strain unharmed by methicillin and other antibiotics. Serving as senior author on the new study was Dr Lloyd Miller, formerly a professor of dermatology, infectious diseases and orthopaedic surgery at the Johns Hopkins University School of Medicine and now with Janssen Research and Development.
Dr Miller said the research team was originally intending to study the mechanisms behind MRSA skin infections in mice with and without the ability to manufacture interleukin-1 beta (IL-1β). This protein, transformed into its active form by enzymes called caspases, enhances protective immunity by helping immune cells called neutrophils, monocytes and macrophages fight bacterial infections.
“We gave the mice a blocker of all caspases [pancaspase inhibitor], a compound known as Q-VD-OPH, thinking it would leave both sets of mice more vulnerable to MRSA infection,” Dr Miller said. “To our surprise, blocking caspases had the opposite effect, resulting in a rapid and remarkable clearing of the MRSA bacteria by keeping the immune cells alive and boosting their protective function.”
Sensing they might have accidentally uncovered a means of fighting bacterial superbugs, Dr Miller and his colleagues conducted their latest study to confirm the unexpected finding was not a fluke. The results, published in the journal Science Translational Medicine, were encouraging.
“A single oral dose of Q-VD-OPH decreased the size of MRSA skin lesions and rapidly cleared the bacteria compared with vehicle-treated [given the carrier solution without Q-VD-OPH] and untreated mice,” said lead author Dr Martin Alphonse, a dermatology postdoctoral fellow at the Johns Hopkins University School of Medicine. “And surprisingly, the treatment worked whether IL-1β was present or not — and without administering any antibiotics.”
The researchers found that the pancaspase inhibitor reduces apoptosis — one of three main methods the body uses to remove worn-out or damaged cells — of neutrophils and monocytes, leaving them in plentiful numbers and better able to remove MRSA bacteria.
“It’s like a fire department where older firetrucks are kept operating to help put out blazes, when otherwise they would have been taken out of service,” Dr Miller said.
The researchers also saw enhanced necroptosis — a second controlled cell death process similar to apoptosis — of macrophages, which are mature monocytes.
“The destruction of macrophages by necroptosis releases [a] large amount of tumor necrosis factor, or TNF, a protein that triggers bacteria-fighting immune cells to swarm into an infected area of skin,” Dr Alphonse said.
Finally, the researchers tested whether Q-VD-OPH in mice could have broader activity against two other dangerous skin bacteria, Streptococcus pyogenes (the cause of multiple diseases, including scarlet fever, necrotizing fasciitis and toxic shock syndrome) and Pseudomonas aeruginosa (often a threat to hospitalised patients on ventilators, with catheters or suffering wounds from surgery or burns). The targeting of the body’s immune system against bacteria via pancaspase inhibition — referred to as ‘host-directed immunotherapy’ — proved just as successful as it had been for MRSA.
“It was an accidental finding by Alexander Fleming that led to the golden age of antibiotics, but now that’s nearing the end because of antibiotic-resistant bacteria,” Dr Miller said. “It seems fitting that another surprise in the lab could be the start of a second golden age, the use of host-directed immunotherapy.”
Please follow us and share on Twitter and Facebook. You can also subscribe for FREE to our weekly newsletters and bimonthly magazine.
Aussie biotech to manufacture mRNA paediatric brain cancer vaccines
A Queensland-based biotechnology company will manufacture personalised mRNA paediatric brain...
Who's afraid of killer whales? — white sharks and prolonged absences
Is killer whale predation the sole driver of white shark long absence? Australian researchers...
Five scenarios for the future of Antarctic life
A team of Australian and international researchers have predicted five possible outcomes for how...




