Bacteriophage cocktail to combat superbugs
Researchers at Monash University and The Alfred are using bacterial viruses, known as bacteriophages, to combat a highly problematic, antimicrobial-resistant bacteria, in a new approach to precision medicine in hospitals battling antimicrobial resistance (AMR). Their breakthrough has been published in the journal Nature Microbiology.
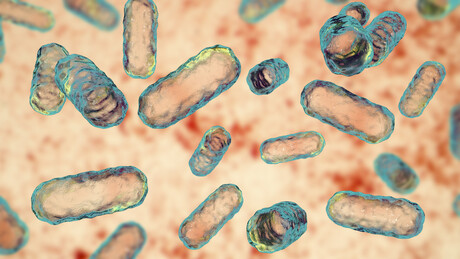
The team’s treatment, named Entelli-02, is a five-phage cocktail designed specifically to target Enterobacter cloacae complex (ECC), a group of bacteria responsible for severe infections. Enterobacter infections have emerged in hospitals around the world and have the capacity to develop resistance to many last-line antibiotics, meaning they are notoriously difficult to treat.
Using a decade’s worth of bacterial isolates, Monash’s Dr Dinesh Subedi said the research team developed and produced Entelli-02 through a rigorous process of phage isolation, genetics and preclinical testing.
“We initially began with three phages in our cocktail, but through iterative design, we improved the cocktail by genetically adapting the viruses to expand their host range, followed by selection of two additional phages with improved treatment outcomes,” said Subedi, who served as lead author on the study.
“The final product, Entelli-02, contains five phages that can kill a broad range of Enterobacter isolates and reduce bacterial loads in infected mice by over 99%.”
“This is the first time we’ve designed and developed a clinical-ready phage therapy product tailored to an AMR bacterial pathogen at a local hospital,” added study leader and senior Professor Jeremy J Barr, from Monash University. “Entelli-02 is not just a scientific achievement; it’s a clinical tool built for frontline use against deadly, drug-resistant, bacterial pathogens.”
Entelli-02 was manufactured as a therapeutic-grade phage product at the Monash Phage Foundry, meeting sterility and safety standards for intravenous use under the Therapeutic Goods Administration Special Access Scheme. The end result, according to co-senior author Professor Anton Peleg from The Alfred and Monash University, is an off-the-shelf product to promptly support the treatment of some of our most difficult infections.
“This is a blueprint for how hospitals can respond to AMR outbreaks with precision therapies,” Barr concluded. “We’re bridging the gap between broad-spectrum antimicrobial treatments and personalised phage therapy to deliver a ready-to-use solution that’s both targeted and scalable.”
AusBiotech and Proto Axiom partner on investor-focused life sciences programs
AusBiotech and Proto Axiom have announced a partnership to strengthen national coordination...
The University of Sydney formalises cervical cancer elimination partnership
The success of a cervical cancer elimination program has led to the signing of a memorandum of...
Noxopharm says paper reveals science behind its immune system platform
Clinical-stage Australian biotech company Noxopharm Limited says a Nature Immunology...




