HIV drugs suppress transmission of a different viral infection
A landmark study from the Walter and Eliza Hall Institute (WEHI) and The Peter Doherty Institute for Infection and Immunity has found that existing HIV drugs can suppress transmission of the life-threatening HTLV-1 virus in mice. Published in the journal Cell, the work could lead to the first treatments to prevent the spread of a virus that is endemic among many First Nations communities around the world.
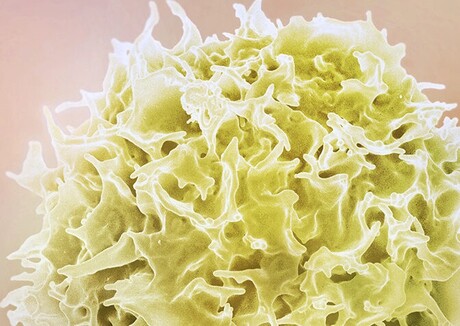
Human T-cell leukaemia virus type 1 (HTLV-1) is a virus that infects the same cell type as HIV — T cells, a type of blood immune cell that helps the body fight off infections. A small proportion of people infected with HTLV-1 after a long duration of infection develop serious diseases, such as adult T-cell leukaemia and spinal cord inflammation. But while around 10 million people globally live with the virus, it remains a poorly understood disease that currently has no preventative treatments and no cure.
“As HTLV-1 symptoms can take decades to appear, by the time a person knows they have the infection the immune damage is already in full swing,” said WEHI Laboratory Head Dr Marcel Doerflinger, co-lead author on the new study.
“Suppressing the virus at transmission would allow us to stop it before it has the chance to cause irreversible damage to immune function, leading to disease and a premature death.”
In a research effort spanning 10 years, the collaborative team isolated the virus and developed a humanised mouse model for HTLV-1 that enabled them to study how the virus behave in a living organism with a human-like immune system. The mice were transplanted with human immune cells that are susceptible to HTLV-1 infections, including Australia’s genetically novel HTLV-1c strain.
Research by co-lead author Professor Damian Purcell, Head of Molecular Virology at the Doherty Institute, isolated the virus from First Nations donors and identified significant genetic differences between the HTLV-1c strains from Central Australia compared to the HTLV-1a strains found internationally. The findings show that both strains caused leukaemia and inflammatory lung disease in the mice, with HTLV-1c showing more aggressive features.
The mice were then treated with tenofovir and dolutegravir — two antiviral therapies currently approved to silence HIV and prevent AIDS. The team discovered both drugs could powerfully suppress HTLV-1, and were equally effective against both strains.
“Our study marks the first time any research group has been able to suppress this virus in a living organism,” Doerflinger said.
“What’s most exciting is that these antivirals are already in use for millions of HIV patients, meaning there’s a direct path for the clinical translation of our findings.
“We won’t have to start from scratch because we already know these drugs are safe and effective. And now we’ve shown that their use can very likely be extended to HTLV-1.”
Furthermore, the team discovered that human cells containing HTLV-1 could be selectively killed when mice were treated with HIV drugs in combination with another therapy inhibiting a protein (MCL-1) known to help rogue cells stay alive. The team is now leveraging precision RNA therapies to develop new ways to target MCL-1 and establish combination treatments that can be clinically tested, which they believe could offer a promising curative strategy for HTLV-1.
The development of the humanised mouse models was spearheaded by lead author Professor Marc Pellegrini, WEHI Honorary Fellow and Executive Director at the Centenary Institute. Pellegrini said the mouse models were not only critical in identifying potential therapeutic targets, they also allowed researchers to understand how different strains of the HTLV-1 virus can alter disease symptoms and outcomes.
“It’s long been hypothesised that differences in viral subtype may influence disease outcomes, but a lack of research into HTLV-1 has made it difficult for us to find the evidence needed to support this claim — until now,” he said.
“Our study provides critical insights that enable us to better understand the consequences of the distinct molecular make-up of the virus affecting our First Nations communities. This will further help us to investigate ways to create the tools needed to control the spread of this virus subtype.”
The research team is currently in talks with the companies behind the HIV antivirals used in this study, to see if HTLV-1 patients can be included in their ongoing clinical trials. If successful, this would pave the way for these drugs to become the first approved pre-exposure prophylaxis against HTLV-1 acquisition.
“Despite Australia’s high burden of HTLV-1, the virus and its associated diseases are still not notifiable in most states and true infection rates in the nation remain unknown,” Purcell said.
“People at risk from HTLV-1 deserve biomedical tools like those that provide game-changing therapeutic and prevention options for other blood-borne persistent viral infections, such as HIV.
“There is a real opportunity to prevent the transmission of HTLV-1 and end the diseases caused by these infections. Our research findings are a major leap forward in this.”
How a tiny worm changed a decade of scientific thinking
A tiny roundworm has helped University of Queensland scientists rethink the way sensory nerve...
A scientist, a cooler and a long-haul flight in the fight against MND
Early in January 2026, neuroscientist Dr Rachael Dunlop boarded a flight from Sydney to the US...
Mini lung organoids could help test new treatments
Scientists have developed a simple method for automated the manufacturing of lung organoids...



