Anti-TB drugs can actually increase risk of TB reinfection
Current treatments for tuberculosis (TB) are very effective in controlling TB infection caused by Mycobacterium tuberculosis (Mtb), but they don’t always prevent reinfection. So why are our bodies unable to generate permanent immunity to TB? Scientists from McGill University may have found the answer in the human gut.
Gut microbiota are critical to keeping us healthy; they help to digest food, combat pathogenic microbes and reinforce our immune system. Recent research has shown that chronic use of antibiotics leads to disruption of this community, which can in turn lead to dysregulation of the immune system. It remains unclear, however, whether changes in the composition of the microbes living in our gut have an influence on TB infection.
To find out, Drs Irah King and Maziar Divangahi from the Research Institute of the McGill University Health Centre (RI-MUHC), with colleagues from McGill’s Macdonald Campus, treated mice with the most commonly used anti-TB drugs — isoniazid, rifampicin and pyrazinamide — for a period of eight weeks. They found that while all three drugs significantly altered the composition of the mice’s gut microbiome, only mice treated with isoniazid combined with pyrazinamide showed an increase in susceptibility to Mtb infection.
Published in the journal Mucosal Immunology, the study results indicate that anti-TB drugs caused changes to gut microbiota, increasing susceptibility to Mtb infection as a result. The researchers confirmed that this susceptibility was due to a compromised gut microbiota by looking at faeces; transplanting faeces from healthy mice into animals treated with anti-TB drugs was sufficient to restore immunity to Mtb.
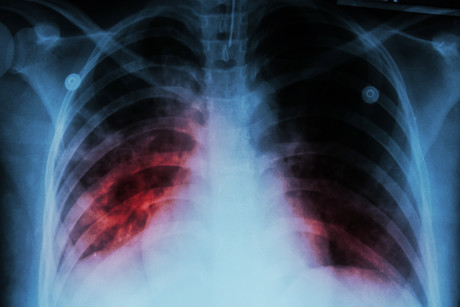
Dr King and his colleagues also wanted to better understand the gut–lung axis — a bidirectional communication system between microorganisms residing in the gastrointestinal tract and the lungs — in order to see how this might be involved in Mtb infection and immunity. To do so, they evaluated a number of lung cell types known to be important for resistance to Mtb infection. Following anti-TB treatment, alveolar macrophages — a type of immune cell located in the airways of mice and humans and the first cell to encounter Mtb upon infection — were compromised in their ability to kill Mtb.
“We need to do more research in order to understand how the microbiome affects alveolar macrophages, because these cells are critical for controlling early TB infection,” Dr King sadi. “We also need to identify the molecular pathways involved in the gut–lung axis.”
Researchers are already thinking of monitoring patients who are being treated with anti-TB drugs to see how their gut microbiota changes over time and once treatment has stopped. The idea will be to control changes to the microbiome in combination with drugs that are effective at killing Mtb.
“Anti-TB therapies have been incredibly efficient in controlling the TB epidemic by decreasing morbidity and mortality associated with Mtb,” Dr King said. “Now, this work provides a basis for novel therapeutic strategies exploiting the gut-lung axis in Mtb infection.”
Please follow us and share on Twitter and Facebook. You can also subscribe for FREE to our weekly newsletters and bimonthly magazine.
argenx and Monash University partner against autoimmune diseases
To advance a pioneering molecule for autoimmune diseases, global immunology company argenx has...
Archer completes potassium sensing alpha prototype
Quantum technology company Archer Materials Limited has developed an early Biochip prototype...
Farm animals and aquaculture cryopreservation partnership announced
Vitrafy Life Sciences Limited has announced that it has entered a 12-month exclusive agreement...



