Bowel cancer drugs tested on tumour organoids
A research team led by the Walter and Eliza Hall Institute (WEHI) has grown tumour organoids in the lab, in order to predict what drugs will work for bowel cancer patients before they begin treatment. A clinical trial is now being developed based on the results, which have been published in the journal Cell Reports Medicine.
While bowel cancer cases can be treated successfully if found early, less than half of all patients are diagnosed at the initial stages due to a lack of symptoms. And while there are an increasing number of treatment options available, there is currently a limited ability to predict which therapy will be most effective for each patient.
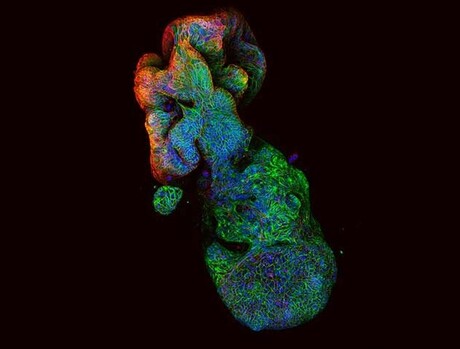
A tumour organoid is a miniature 3D model of a cancer that is the size of a grain of sand. Grown in a laboratory from a patient’s own tissue sample, tumour organoids mimic the characteristics of the cancer from which they were created, including sensitivity to drug treatment.
WEHI researchers have now shown that the technology can identify the most effective treatment for individual bowel cancer patients — by assessing how their organoids responded to specific drugs — in a breakthrough that could end the current trial-and-error process that goes into selecting a cancer treatment for patients. And as hundreds of organoids can be grown from one patient tissue sample, it is possible to test a wide range of different therapy options in the laboratory.
“Each time you give a patient an ineffective treatment, you lose 2–3 months on something that won’t work,” said co-lead researcher Professor Peter Gibbs.
“The window for successful treatment is often limited, so it is vital that we choose the options with the highest chance of success and avoid other treatments that are unlikely to work.
“Many patients with advanced bowel cancer only get one or two chances at treatment. Knowing what is most likely to work before they start treatment would make a significant difference to their survival outcomes and quality of life.”

As part of the new study, the organoids of 30 patients with advanced stages of bowel cancer were used to pre-test chemotherapy drugs in a clinical feasibility trial. According to corresponding author Associate Professor Oliver Sieber, organoid drug testing was able to predict treatment responses for study patients with a notable 83% accuracy, validating over five years of research in the process.
“If a drug had no effect on the tumour organoid, then this treatment would also have no effect on the patient — and vice versa,” Sieber said.
“Importantly, pre-testing showed the therapies that won’t work with over 90% accuracy.”
Researchers also used the organoids to test the effectiveness of chemotherapy drugs that are not commonly used for bowel cancer patients. They found two patient organoids were sensitive to a drug that is often used for breast and bladder cancers.
“Not only did we show that organoid drug testing could, for the first time, predict patient responses to bowel cancer treatment, we also managed to find a new therapeutic option for patients in our trial,” Sieber said.
“That is the power of this incredible technology.”
The study is now being translated into a clinical trial that will open at multiple Victorian hospitals this year.
AusBiotech and Proto Axiom partner on investor-focused life sciences programs
AusBiotech and Proto Axiom have announced a partnership to strengthen national coordination...
The University of Sydney formalises cervical cancer elimination partnership
The success of a cervical cancer elimination program has led to the signing of a memorandum of...
Noxopharm says paper reveals science behind its immune system platform
Clinical-stage Australian biotech company Noxopharm Limited says a Nature Immunology...




