BRCA1 gene mutation may increase risk of impaired fertility
People with a BRCA1 gene mutation, which increases breast and ovarian cancer risk, are also at increased risk of impaired fertility. That’s according to new research led by Monash University, conducted in preclinical models and human tissue samples and published in the journal eBioMedicine.
The BRCA1 and BRCA2 genes protect against breast and ovarian cancer, and a mutation of either gene increases the risk of developing cancer. But while previous preclinical models have indicated that partial loss of BRCA1 function may reduce egg numbers in the ovary, Professor Karla Hutt from the Monash Biomedicine Discovery Institute noted that the potential impacts of complete loss of BRCA1 function on egg number and fertility “had never been studied”.
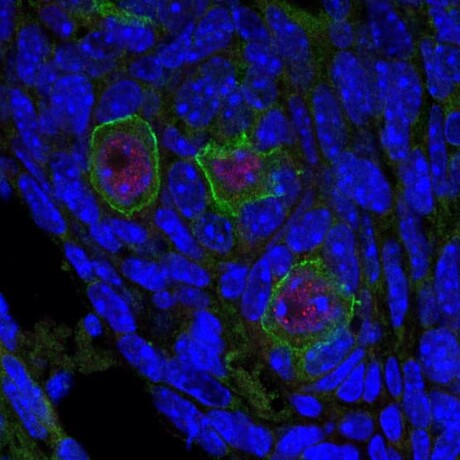
As part of the new study, mice were bred with no BRCA1 gene in their eggs, which models a BRCA1 gene mutation causing complete loss of BRCA1 function. While the mice’s fertile lifespan length was not altered, the mutation led to reduced litter sizes, egg quality and egg numbers — particularly with advancing age. Egg maturation rates were also decreased by 45% in reproductively aged mice lacking BRCA1.
“The data show that BRCA1 is important for maintaining egg number, quality and fertility,” said Hutt, who is a senior author on the study.
In women, measuring anti-Müllerian hormone (AMH) levels in blood is considered the gold-standard indirect marker of the number of eggs they may have. However, when the researchers analysed AMH levels and estimated egg numbers from ovarian tissues of a small number of women with a BRCA mutation, they saw no correlation between these measures. This suggests that more studies are needed to better understand if AMH is a good predictor of egg numbers in women with a BRCA mutation.
Co-first author Dr Amy Winship, from the Hutt Laboratory, said the study extended knowledge of BRCA1’s critical role in maintaining fertility.
“This has implications for women who carry BRCA mutations to make considered family-planning and possibly fertility-preservation decisions, like egg freezing,” Winship said.
“Additionally, since these women are already at higher risk of developing breast and ovarian cancer during their lifetime, they are more likely to receive fertility-damaging cancer treatments.”
Co-first author Dr Lauren Alesi, also from the Hutt Laboratory, said future studies are needed to understand the impacts of cancer treatments on fertility in the context of BRCA mutations.
“Because fertility may already be reduced, having a BRCA mutation and receiving cancer treatments could worsen the fertility-damaging effects of these treatments,” Alesi said. “Further research in our preclinical models and patient samples will help us to determine this.”
Co-author Leslie Gilham, herself a breast cancer survivor, said the research provides the evidence needed to support young women who have either a BRCA1 mutation or breast cancer.
“It has the potential to be practice changing and address one of the significant unmet needs in this young group of patients,” she said.
argenx and Monash University partner against autoimmune diseases
To advance a pioneering molecule for autoimmune diseases, global immunology company argenx has...
Archer completes potassium sensing alpha prototype
Quantum technology company Archer Materials Limited has developed an early Biochip prototype...
Farm animals and aquaculture cryopreservation partnership announced
Vitrafy Life Sciences Limited has announced that it has entered a 12-month exclusive agreement...



