Cardiac organoids bring hope for treating heart disease
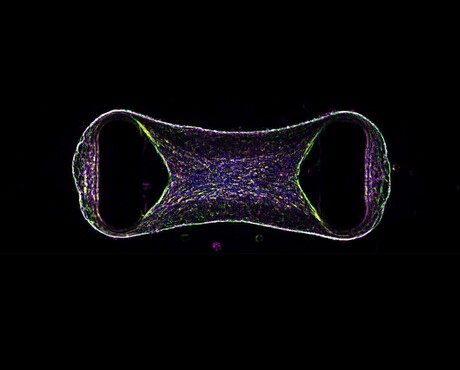
Scientists from QIMR Berghofer’s Cardiac Bioengineering Lab have developed lab-grown, three-dimensional heart tissues known as cardiac organoids that mimic the structure and function of real adult human heart muscle. Published in the journal Nature Cardiovascular Research, their work is expected to bring us closer to understanding and treating heart disease — especially in children.
To create the tissues, the researchers used special cells called human pluripotent stem cells, which can turn into any cell in the body. When these stem cells become heart cells, they usually stay immature and more like the heart tissue found in a developing baby, which can limit their usefulness to model diseases that present in childhood or as an adult.
The researchers activated two key biological pathways to mimic the effects of exercise and mature these cells, making them behave more like genuine adult heart tissue despite measuring no more than the size of a chia seed. This breakthrough means scientists can now use these lab-grown heart tissues to test new drugs that could help people with heart conditions.
“There’s huge benefit to studying heart diseases in this way,” said QIMR Berghofer’s Professor James Hudson. “Using human cardiac organoids allows us to screen many more compounds, speeding up the process of drug development.”
The researchers also modelled types of heart disease caused by certain mutations in genes called ryanodine, calsequestrin and desmoplakin. In particular, Desmoplakin (DSP) cardiomyopathy has traditionally been hard to study; however, the team was able to recreate key features of the disease using the lab-grown heart tissues. Hudson said the results were promising on several levels.
“In the cardiac organoids, the disease caused scarring (fibrosis) and made the tissue pump less effectively — similar to what happens in patients’ heart disease,” Hudson said. “We then tested a new type of drug called a bromodomain and extra-terminal protein inhibitor, and found this medication improved the heart tissue’s function.”
The Murdoch Children’s Research Institute (MCRI) and The Royal Children’s Hospital played a key part in the research by providing advanced gene and protein analysis, and modelling heart disease using samples from the Melbourne Children’s Heart Tissue Bank. MCRI Associate Professor Richard Mills says the team’s findings will speed up the process of identifying treatments to improve heart function.
“Our approach allows us to more accurately model childhood heart conditions, to ultimately find better treatments for some of the sickest people in our community,” he said. “The collaboration with QIMR Berghofer and The Royal Children’s Hospital is accelerating progress towards these goals, and this approach has the potential to be used across a whole spectrum of childhood heart disease.”
AusBiotech and Proto Axiom partner on investor-focused life sciences programs
AusBiotech and Proto Axiom have announced a partnership to strengthen national coordination...
The University of Sydney formalises cervical cancer elimination partnership
The success of a cervical cancer elimination program has led to the signing of a memorandum of...
Noxopharm says paper reveals science behind its immune system platform
Clinical-stage Australian biotech company Noxopharm Limited says a Nature Immunology...




