Immune cell boost could enable lasting vaccine protection
A research team led by the Walter and Eliza Hall Institute (WEHI) has found a promising new way to enhance the effectiveness of vaccines by tapping into the potential of a specific type of immune cell, pointing to a future where more diseases are vaccine-preventable and treatable, and where regular vaccine boosting is no longer needed. Their work has been published in the Journal of Experimental Medicine.
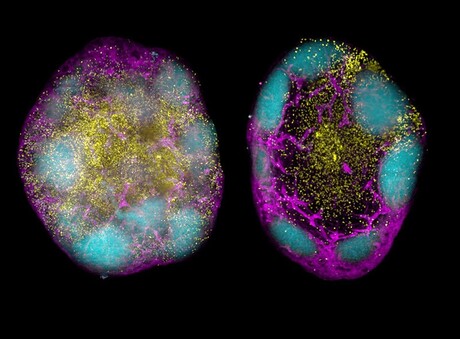
Despite being the most effective preventative medicine in history, vaccines often rely on antibodies for immune protection, which naturally fade over time. Furthermore, in the case of rapidly mutating viruses like influenza and COVID-19, we need to be able to target any newly circulating variants. The research team has now uncovered a way to enhance stem cell-like memory CD8+ T cells following vaccination, showing exceptional promise at overcoming these two obstacles.
“We’ve believed for some time that stem cell-like memory CD8+ T cells correlate with long-lasting protection, and this study is the first to prove this benefit,” said WEHI Immunology Division Head Associate Professor Joanna Groom, lead author on the new study.
Stem cell-like CD8+ T cells have a remarkable self-renewing capacity and can remember threats for years or even decades. The research team harnessed immunomodulation, to adjust immune responses at the cellular level, alongside mRNA vaccine technology to promote the generation of these potent cells in mice. mRNA vaccines, like those used to protect against COVID-19, are highly adaptable and can be quickly generated to tackle new and emerging viral threats, making them a highly promising tool for vaccine development.
“The results are really striking — we were incredibly excited at how effective our new vaccine strategy was at boosting these cells,” Groom said.
“Our approach has the potential to reduce the need for frequent booster shots, while maintaining strong and lasting immunity.
“Inducing these stem cell-like memory CD8+ T cells is the next big challenge for improving vaccines, and we’re energised to bring this future closer.”
In addition to viruses, increased numbers of these cells are associated with improved cancer outcomes. First author Benjamin Broomfield, a PhD student at WEHI, said this indicated that the findings could inform new cancer immunotherapies.
“We know the body needs these cells to eliminate cancerous cells and our lab is now focused on applying the approach used in this study to boost stem cell-like CD8+ T cells to tackle cancer,” Broomfield said.
“A therapeutic vaccine for cancer would be a total game changer, and we’re optimistic about where this research can go.”
AusBiotech and Proto Axiom partner on investor-focused life sciences programs
AusBiotech and Proto Axiom have announced a partnership to strengthen national coordination...
The University of Sydney formalises cervical cancer elimination partnership
The success of a cervical cancer elimination program has led to the signing of a memorandum of...
Noxopharm says paper reveals science behind its immune system platform
Clinical-stage Australian biotech company Noxopharm Limited says a Nature Immunology...




