Extra oxygen could overcome radiotherapy resistance in tumours
For most of our tissues and cells, a lack of oxygen, or hypoxia, is bad news. Cancer cells, on the other hand, can thrive in these conditions, which render tumours less susceptible to anticancer treatments including radiation. Now researchers have found a way to break through cancer’s hypoxia-induced defences, which they have published in the journal Pharmaceutics.
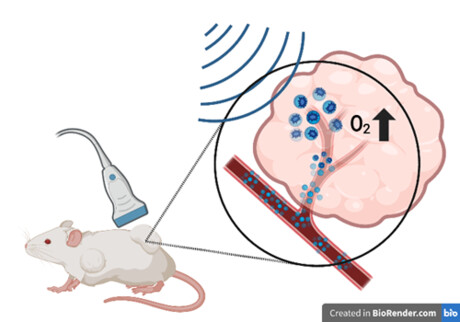
A longstanding staple of cancer management, radiation therapy sees clinicians use high doses of radiation to kill cancer cells. But many tumours are resistant to radiotherapy, and hypoxia is one of the major reasons why. With this in mind, a research team led by Thomas Jefferson University and Drexel University devised a strategy that combines ultrasound with microbubbles to deliver both oxygen and cancer drugs to tumours.
“Whenever I say we’re delivering oxygen to tumours, a lot of people say, ‘Well that’s crazy, you’re going to encourage them to grow’,” said study co-author Margaret Wheatley, a professor of biomedical engineering at Drexel University. But radiation therapy, which prevents cancer cells from replicating, requires an ample supply of oxygen close by to be effective, she explained.
Seeking to beat radiotherapy resistance, Wheatley and colleagues designed a method that sensitises tumours to radiotherapy using tiny, delicate bubbles that are about the size of red blood cells. To increase oxygen levels in tumours, they packaged oxygen molecules into the microbubbles. To prevent cancer cells from consuming the oxygen for their own benefit, they also added the drug lonidamine, which interrupts cancer cell metabolism.
After assembly, the microbubbles are injected and circulate throughout the body, only releasing their payload at the intended target, sparing healthy tissues. The trick to the targeted release is ultrasound. By specifically casting ultrasound waves at a tumour, the researchers can cause the microbubbles that have travelled there to pop and release their contents.
In a previous study, the researchers used the method to treat mice with tumours derived from breast cancer cells, producing favourable results. Here they upped the ante, working against head and neck cancer cell-derived tumours — which are more hypoxic than other solid tumours and also relatively resistant to radiation therapy.
The researchers injected mice with microbubbles containing oxygen and lonidamine, bursting them at the tumour site with ultrasound, while also administering a drug called metformin — known to slow cancer growth — orally. Other groups of mice were given less than the full treatment, not receiving one or many of the elements of the strategy prior to radiotherapy.
After exposing the animals to radiation, the researchers tracked the size of the tumours over the following three months and found that all groups that received some degree of treatment saw varying levels of slowed tumour growth. Mice treated with fully loaded bubbles and metformin prior to radiotherapy lived the longest, their tumour growth slowing drastically. According to the authors, the increase in oxygen within the tumours made them more vulnerable to radiation treatment.
Eisenbrey said that gaining ground on head and neck cancer is a very encouraging result, even in mice. The team now intends to continue fine-tuning the method by optimising radiation and drug doses for better results and streamlining microbubble fabrication, ultimately bringing their solution closer to reality for human patients.
Babies of stressed mothers likely to get their teeth earlier
Maternal stress during pregnancy can speed up the timing of teeth eruption, which may be an early...
Customised immune cells used to fight brain cancer
Researchers have developed CAR-T cells — ie, genetically modified immune cells manufactured...
Elevated blood protein levels predict mortality
Proteins that play key roles in the development of diseases such as cancer and inflammation may...



