Light therapy eliminates antibiotic-resistant superbugs
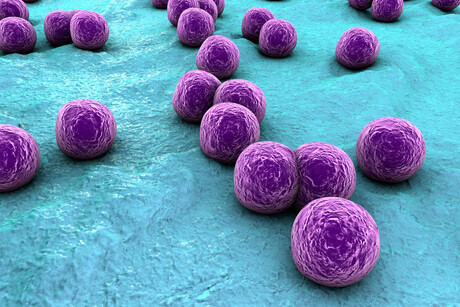
Light-activated nanotechnology, developed at the University of South Australia (UniSA), has the potential to eradicate some of the most notorious and potentially deadly bacteria in the world. Researchers tested their antimicrobial photodynamic therapy on recalcitrant bacterial infections caused by antibiotic-resistant strains of golden staph and Pseudomonas aeruginosa, with their results published in the journal Pharmaceutics.
Golden staph (Staphylococcus aureus) and P. aeruginosa are among the most deadly superbugs in the world. As noted by lead researcher Dr Muhammed Awad, “Golden staph and Pseudomonas aeruginosa are both highly transmissible bacteria, commonly found on people’s skin. But if they get into the blood, they can lead to sepsis or even death.
“Patients in hospitals — particularly those with wounds or catheters, or those on ventilators — have a higher risk of getting these bacteria, and while antibiotics may help, their extensive use has led to waves of microbial resistance, often making them ineffective.
“Our photodynamic technology works differently, harnessing the energy of light to generate highly reactive oxygen molecules that eradicate microbial cells and kill deadly bacteria, without harming human cells.”
The new light therapy was found to eliminate golden staph and P. aeruginosa by 500,000-fold and 100,000-fold respectively. According to senior researcher Professor Clive Prestidge, this is because the technology has some key advantages over conventional antibiotics and other light therapies.
“The new therapy is created in an oil that that is painted on a wound as a lotion,” Prestidge said. “When laser light is applied to the lotion, it creates reactive oxygen species which act as an alternative to conventional antibiotics.
“Current photoactive compounds also suffer from poor water solubility, which means that they have limited clinical application.
“Our approach uses food-grade lipids to construct nanocarriers for the photoactive compound, which improves its solubility and antibacterial efficiency far beyond that of an unformulated compound.
“These molecules target multiple bacterial cells at once, preventing bacteria from adapting and becoming resistant. So it’s a far more effective and robust treatment.
“Importantly, the human skin cells involved in the wound-healing process showed enhanced viability, while the antibiotic-resistant bacteria were entirely eradicated.”
With the technology now gaining the attention of scientists worldwide, Prestidge said the next step is to commence clinical trials and develop the light therapy further to be available in clinics. “With the support of funding bodies, we hope that Australians will have access to this technology as soon as possible,” he said.
Portable point-of-care test detects four common STIs in under an hour
Australian researchers have developed a portable point-of-care test that detects four common...
AusBiotech and Proto Axiom partner on investor-focused life sciences programs
AusBiotech and Proto Axiom have announced a partnership to strengthen national coordination...
The University of Sydney formalises cervical cancer elimination partnership
The success of a cervical cancer elimination program has led to the signing of a memorandum of...




