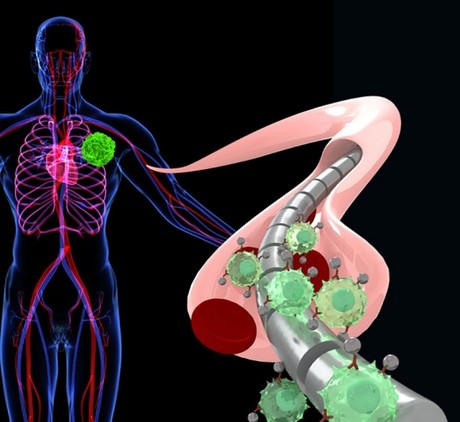
How a magnetised wire attracts tumour cells
Stanford scientists have used a magnetic wire to capture free-floating tumour cells in the blood.
The technique, which has only been used in pigs so far, is claimed to attract from 10–80 times more tumour cells than current blood-based cancer-detection methods, making it a potent tool to catch the disease earlier.
The wire, which is threaded into a vein, attracts special magnetic nanoparticles engineered to glom onto tumour cells that may be roaming the bloodstream if you have a tumour somewhere in your body. With these tumour cells essentially magnetised, the wire can lure the cells out of the free-flowing bloodstream using the same force that holds family photos to your refrigerator.
Sanjiv “Sam” Gambhir, MD, PhD, professor and chair of radiology and director of the Canary Center at Stanford for Cancer Early Detection, developed the wire with the help of his colleagues. “It could be useful in any other disease in which there are cells or molecules of interest in the blood,” said Gambhir. “For example, let’s say you’re checking for a bacterial infection, circulating tumour DNA or rare cells that are responsible for inflammation — in any of these scenarios, the wire and nanoparticles help to enrich the signal, and therefore detect the disease or infection.”
The study was published in Nature Biomedical Engineering. Gambhir is the senior author. Postdoctoral scholar Ophir Vermesh, MD, PhD; surgery resident Tianjia Jessie Ge, MD; and MD-PhD student Amin Aalipour share lead authorship.
No vial of blood necessary
Cells that have sloughed off the tumour and cruise the bloodstream freely, otherwise known as circulating tumour cells, can serve as cancer biomarkers, signalling the presence of the disease.
“These circulating tumour cells are so few that if you just take a regular blood sample, those test tubes likely won’t even have a single circulating tumour cell in them,” said Gambhir, the Virginia and D.K. Ludwig Professor of Clinical Investigation in Cancer Research. It would be like searching for a grain of sand in a bathtub, but only scooping out a few cups of water.
That is where the magnetic wire can make a difference, according to Gambhir. For the wire, which is about the length of the little finger and the thickness of a paperclip, to work, circulating tumour cells must be effectively magnetised with nanoparticles. The nanoparticles contain an antibody that latches onto circulating tumour cells. Once the floating tumour cell and nanoparticle are hitched, the cell lugs the tiny magnet around with it, and when the cell-magnet complex flows past the wire, it’s compelled by magnetic force to veer from its regular path in the bloodstream and stick to the wire. Then, the wire is removed from the vein and the cells are stripped for analysis.
Gambhir and his team have yet to try out the wire in people, as they still have to file for approval from the Food and Drug Administration, but they have successfully tested it in pigs, placing the device in a vein near the pig’s ear. That vein is fairly similar to veins in the human arm.
“We estimate that it would take about 80 tubes of blood to match what the wire is able to sample in 20 minutes,” Gambhir said. Of course, he continued, it’s not practical to remove 80 test tubes of blood from one person; that’s more than a half-litre. “So, we’re hoping this approach will enrich our detection capability and give us better insight into just how rare these circulating tumour cells are, and how early on they exist once the cancer is present.”
A flexible wire
Gambhir said the technique could also be used to gather genetic information about tumours located in hard-to-biopsy places or to provide information about the efficacy of a cancer treatment. Perhaps most intriguingly, the magnetic wire may even stand to evolve into a treatment in and of itself.
It could be useful in any other disease in which there are cells or molecules of interest in the blood. Now, Gambhir is working to ready the technique for humans, which involves approval for the nanoparticles. His lab is conducting toxicity studies in mice, paying close attention to what happens to leftover nanoparticles that don’t bind. So far, there are no signs of toxicity, and the extras decay over the course of a few weeks, he said. Gambhir is also looking into nanoparticles that are already FDA-approved, working to tweak them for use with the wire. Once approved for humans, the goal is to develop the technology into a multipronged tool that will boost detection, diagnosis, treatment and evaluation of cancer therapy.
The study’s other Stanford authors are veterinary research coordinator Yamil Saenz, DVM; former graduate students Chin Chun Ooi, PhD, and Yue Guo, PhD; radiology and molecular imaging scientist Israt Alam, PhD; senior research scientist Seung-min Park, PhD; graduate student Charlie Adelson; postdoctoral scholars Hamed Arami, PhD, and Yoshiaki Mitsutake, PhD; assistant professor of comparative medicine Jose Vilches-Moure, DVM, PhD; life science technician Elias Godoy; research scientist Michael Bachmann, MD, ScD; preclinical laboratory managing director Jennifer Lyons; instructor of radiology Kerstin Mueller, PhD; life science technician Alfredo Green; Shan Wang, PhD, professor of materials science and engineering and of electrical engineering; and chemistry professor Edward Solomon, PhD, who is also a professor of photon science at SLAC National Accelerator Laboratory.
Gambhir is a member of Stanford Bio-X, the Stanford Cancer Institute, the Stanford Cardiovascular Institute and the Stanford Neurosciences Institute.
The study was funded by the National Institutes of Health (grants U54CA151459, R21CA185804 and S10 RR026714), the Canary Foundation and the Ben and Catherine Ivy Foundation.
Stanford’s Department of Radiology also supported the work.
argenx and Monash University partner against autoimmune diseases
To advance a pioneering molecule for autoimmune diseases, global immunology company argenx has...
Archer completes potassium sensing alpha prototype
Quantum technology company Archer Materials Limited has developed an early Biochip prototype...
Farm animals and aquaculture cryopreservation partnership announced
Vitrafy Life Sciences Limited has announced that it has entered a 12-month exclusive agreement...



